Every week, scientific journals publish dozens of papers pertaining to cannabis, cannabinoids, and the endocannabinoid system. And the pace of research is accelerating.
Between 2018 and 2020, the number of papers mentioning cannabidiol (CBD) nearly doubled from 788 to 1,408. And at the current rate, this year will see another large increase with approximately 1,800 papers referencing CBD published.
Include THC and that projection balloons to nearly 2,600. Then there are the minor cannabinoids, the endocannabinoids, the cannabinoid receptors throughout the human body, and the many constituents of the broader “endocannabidiome.” It’s enough to overwhelm even active researchers venturing beyond their niche in the rapidly expanding field of cannabinoid science – let alone consumers and health professionals.
Real-World CBD Evidence
Relatively few of these papers describe studies conducted with human beings. Many present results from experiments in animals (typically rats, mice, or zebrafish), and some are even more theoretical and removed from the results with which we’re most concerned, those pertaining to actual human health outcomes.
People with moderate or severe symptoms experienced less pain, anxiety, and depression, and greater wellbeing after three months of CBD treatment.
A new paper out of Canada caught our eye because it evaluated a range of outcomes among a large number of patients at a medical cannabis clinic in Quebec (279, to be exact) who had used both CBD and THC in the course of their daily lives over a period of up to six months.
Published in the Journal of Cannabis Research, the paper includes some intriguing results – with the important caveat (common to all real-world or “naturalistic” observational studies due to the lack of a control group) that a cause-effect relationship cannot be inferred.
Compared to their scores at baseline, participants with moderate or severe symptoms reported experiencing considerably less pain, anxiety, and depression, and greater wellbeing, after three months of formal treatment. After six months, the improvements held relatively steady. However, these improvements were not seen in participants categorized as having only mild symptoms.
Due to the subjective, self-reported nature of symptom assessment, the researchers note that findings may be biased by participants’ positive expectation of treatment, which can lead to a placebo effect. But this doesn’t explain why patients with moderate or severe symptoms would respond so much more than those with mild symptoms. “The results of this study contribute to address the myths and misinformation about CBD treatment and demand further investigation,” the authors conclude.
Better Together: Ketamine and CBD
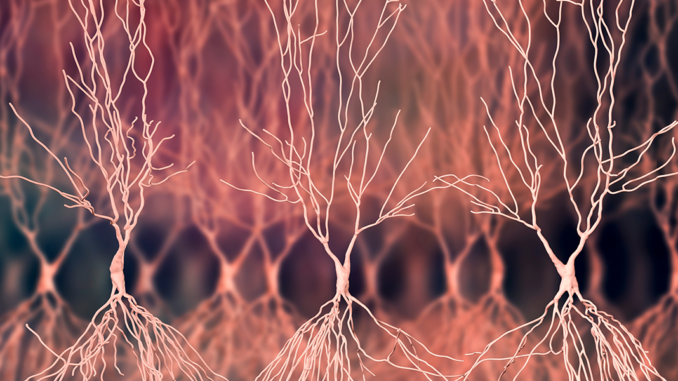
Ketamine and CBD both exert effects that are mediated by the endocannabinoid system. What happens when they are administered together?
An anesthetic with dissociative and hallucinogenic effects, ketamine has of late been increasingly used as a remedy for major depressive disorder at numerous clinics in the US. Scientists based in Brazil and Denmark wanted to ascertain whether CBD, also known for its antidepressant properties, could reduce the unwanted psychostimulant side effects of ketamine.
To find out, the researchers administered ketamine and CBD to mice, both alone and in combination. Their results, reported in Neuropharmacology, indicate that CBD maintained the desired anti-depressant effect of ketamine (according to a behavioral model meant to approximate what we call “depression” in humans), while attenuating ketamine’s adverse stimulant effects (according to an animal model of “locomotor activity”).
The authors stress that these findings will need to be replicated in other animal models. But they also point out there’s good reason to believe they’ll hold. We already know from both human and animal studies that CBD can prevent some of the less desirable effects of other compounds, including cannabidiol’s occasionally brash sibling, THC.
Intergenerational Effects of Omega-3’s
Earlier this year, Project CBD wrote about how the balance of omega-3 and omega-6 fatty acids in one’s diet impacts overall health via the endocannabinoid system (ECS). A recent report by researchers from Brazil, Italy, and Canada in the Journal of Nutritional Biochemistry presents evidence that advances our understanding of the link between these essential dietary compounds and the ECS.
Changes in levels of endocannabinoids and cannabinoid receptors linked to dietary intake of omega-3 fatty acids can be passed from one generation to the next.
Female rats were fed one of three different diets – high in omega-3, low in omega-3, or a control – 15 days before mating and during pregnancy. Then the scientists analyzed the cerebral cortex and hippocampus of both mothers and offspring within a couple days of birth.
Consistent with what would be expected, the researchers found reduced expression of the CB1 cannabinoid receptor and increased expression of the CB2 receptor in the mothers fed an omega-3-deficient diet. Interestingly, they also found the exact same thing in these mother rats’ offspring.
What’s more, in the offspring of mothers fed supplemental omega-3, the researchers found increased levels of the omega-3-derived endocannabinoids DHEA and EPEA in both the hippocampus and the cerebral cortex, as well as reduced levels of the omega-6-derived endocannabinoid 2-AG in the cerebral cortex.
Together these findings demonstrate that changes to levels of endocannabinoids and cannabinoid receptors in the brain associated with dietary intake of omega-3 fatty acids are capable of being passed from one generation to the next – at least in rats. The study does not link these alterations to any specific health outcomes.

BPA, Obesity, and the CB1 Receptor
Now on to zebrafish. These tiny swimmers are commonly used as an animal model in place of mice and rats to better understand human biological systems. (And yes, they do have stripes.)
A team of researchers from three different institutions in China exposed adult male zebrafish to the notorious plastic additive BPA and a related bisphenol, TBBPA, at concentrations commonly found in the environment. Subsequent analyses revealed that these toxic chemicals increased appetite and induced obesity through activation of the CB1 receptor, and that at least four additional bisphenols are also capable of successfully binding to CB1.
Published in the Journal of Hazardous Materials, these findings agree with data discussed in a May 2020 Project CBD article noting that endocrine-disrupting chemicals – including bisphonols, phthalates, parabens, PFAS, and organophosphate pesticides – appear to exert at least some of the their myriad harmful effects on human health through disruption of the endocannabinoid system.
Nate Seltenrich, an independent science journalist based in the San Francisco Bay Area, covers a wide range of subjects including environmental health, neuroscience, and pharmacology.
Copyright, Project CBD. May not be reprinted without permission.



Be the first to comment